The Potential Economic and Public Health Impact of MDMA-Assisted Group Therapy for PTSD in Ukraine
-
23 September 2025Переглянуто: 1238
by Elliot Marseille, Olga Chernoloz, Oleh Orlov
From: https://onlinelibrary.wiley.com/doi/10.1002/wmh3.70039
ABSTRACT
The war in Ukraine has led to widespread trauma, with 6.4 million people suffering from severe, chronic posttraumatic stress disorder (PTSD).
- Assuming a 3-year efficacy, treating 1,000 patients with MAT would cost $1.1 million, prevent 19.2 deaths, and gain 717 quality-adjusted life years (QALYs). .
- From a healthcare payer perspective, the incremental cost-effectiveness ratio (ICER) is $1,537 per QALY gained, with a net monetary benefit (NMB) of $2,843. This indicates that MAT is a cost-effective treatment.
- From a partial societal perspective, MAT generates net savings of $2.6 million for 1,000 patients.
- If scaled to 50% of the eligible patient population over 10 years, MAT could save 48,000 lives and gain 1.5 million QALYs, with net societal savings of $5.6 billion. .
Background
Prevalence of Mental Health Issues: Due to the war, it's estimated that around 9 million Ukrainians will suffer from mental health disorders, with about 2 million experiencing severe disorders. (Martsenkovskyi et al. 2024; World Health Organization 2023)
Challenges with Current Treatments: Over 50% of patients do not respond to or only have a mild, temporary improvement from existing PTSD treatments. (Haviland et al. 2016; Kessler et al. 2005; Savoca and Rosenheck 2000)
MDMA-Assisted Therapy (MAT) Efficacy: In a Phase 3 clinical trial, 67% of MDMA recipients no longer met the criteria for PTSD after treatment, compared to 32% of those who received a placebo. (Mitchell et al. 2021)
Economic Impact of Mental Health: Mental health disorders have significant economic costs through reduced productivity and increased healthcare expenses. The mental well-being of the population is directly linked to the country's recovery and resilience. (World Health Organization 2023)
Cost-Effectiveness of MAT (US studies): A study in the US found that treating 1,000 patients with MAT at a cost of $11,537 per patient would generate discounted net healthcare savings of $9.8 million over 5 years. It would also lead to 1,158 quality-adjusted life years (QALYs) and avert 14.2 premature deaths. (Marseille et al. 2022)
Group Therapy as a Solution: A group therapy format has been proposed to address Ukraine's shortage of mental health professionals. In the U.S., group MDMA therapy for veterans reduced clinician costs by 50.9%, nearly doubling treatment capacity. (Marseille et al. 2023)
Materials and Methods
Researchers used a computer model to figure out the costs and benefits of using MDMA-assisted therapy (MAT) for 1,000 patients in Ukraine. This model, which is based on an earlier study (Marseille et al. 2022), helps to predict how the treatment would affect patients over time.
Who was studied?
The model used data from a real-world Phase 3 study of 90 patients who received MAT between 2018 and 2020. This allowed the researchers to create a realistic picture of how PTSD severity changes after treatment. (Mitchell et al. 2021)
The "Markov Model":
The study used a type of model called a "Markov model" to track patients' health. This model places patients into different levels of PTSD severity (from "asymptomatic" to "extreme") and then predicts their journey through these different health states over time.
- Health and well-being:They used information from patient questionnaires, specifically the EQ-5D-DL, to measure the value of a patient's health. This allows them to calculate "quality-adjusted life years," or QALYs, which combine both the length and quality of life into a single number.
- Costs: They factored in many costs, including medical expenses, lost productivity, and the cost of care for family members. These costs were adjusted to reflect the economic realities in Ukraine, including local salaries and other expenses like lab tests.
- Mortality: The model also included the risk of premature death associated with different levels of PTSD severity.
The study looked at the results from three different points of view:
- Healthcare Payer: Just the direct healthcare costs.
- Societal (limited): Adds in productivity gains and reduced caregiver costs.
- Societal (full): Includes everything from the "limited societal" view, plus the economic gains from preventing premature deaths.
Patient Characteristics
The study on which MAT efficacy is based involved 90 individuals (44 placebo; 46 MDMA) with an average PTSD duration of 14.1 years and a severe to extreme severity level, based on the CAPS-5 scale average score of 44.1. The mean age in the MDMA group was 43, with 58.7% females and 84.9% whites. Most had tried various PTSD treatments, including SSRIs, CBT, EMDR, and other therapies, with only 2.2% not having any prior therapy (Mitchell et al. 2021).
Outcomes
We report per-patient cost of MAT, premature deaths averted, QALYs gained, and net costs or savings from the healthcare payer’s view and two societal perspectives: one including productivity and caregiver costs, and another adding economic losses from premature death. Cost-effectiveness is measured mainly as Net Monetary Benefit (NMB), calculated as incremental benefit times Willingness to Pay (WTP) minus incremental cost. Unlike the incremental cost-effectiveness ratio (ICER), NMB puts costs and benefits on the same monetary scale, making it more useful here since MAT often yields both health gains and savings. ICER is reported only when MAT is not the dominant option.
Treatment Effects
The model used trial outcomes around 8 weeks after the last MDMA session, comparing the active treatment group's pre and posttreatment states without assuming any treatment change for the control. It reflects the intervention's impact by showing the shift in severity distribution, with patient severity categories and their accompanying mortality rates and utilities maintained from trial end without additional change during the analyses period. Details are provided elsewhere (Marseille et al. 2022).
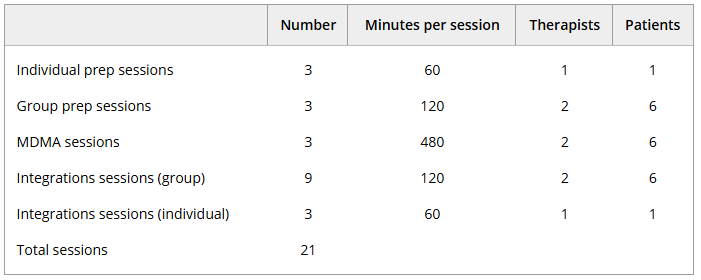
Treatment Protocol
The MAPS phase 3 trial on which the present study's efficacy estimate is based, consisted of the following protocol: After initial assessments and three nondrug therapy sessions, participants were given placebo or MDMA in each of three treatment sessions, followed by three psychotherapy integration sessions after each (a total of nine integration sessions). Trained professionals conducted the therapy with a ratio of two therapists to one study participant for each drug- and nondrug session. Details are provided elsewhere (Mitchell et al. 2021).
Considering the acute shortage of therapists, the introduction of group therapy for MDMA is being pursued in Ukraine. We therefore costed a modified version of this protocol that is organized around three MDMA sessions, and includes a mix of individual and group therapy sessions with a combined total of 21 sessions. Individual therapy sessions consist of one therapist and one patient; and group sessions consist of two therapists and six patients. MDMA treatment regimen consists of the following: Each patient receives six 60-min preparatory sessions before any MDMA session, three individual and three group sessions. The three MDMA sessions that follow are in the group format. Each of these MDMA sessions is followed by four integration sessions, three in group format and one individual session for a total of 12 integration sessions. See Table 1.
Cost of MAT
We used a standard micro-costing approach to estimate the variable cost of delivering MAT per patient served (Muenning 2002). Each of the elements of the therapy were quantified and assigned a cost. For example, clinician costs are the product of the compensation rate including fringe benefits of each clinician multiplied by the number of hours of each clinician required to deliver the therapy and summed across all clinicians and therapy sessions. In addition, we assessed the cost of screening and testing, and the MDMA itself (Maryna Mormul 2023). We then added 10% to the cost of all of the variable cost elements mentioned above to reflect the incremental MAT-related overhead and administration. See Supporting Information: Appendix S1 for details on the estimation of overhead costs.
Excess Healthcare Costs of PTSD
We estimated excess healthcare costs of PTSD using a 2020 European review (von der Warth et al. 2020). A regression model linked per-patient PTSD costs to national healthcare spending. For Ukraine, adjusted per capita spending in 2022 was $1181, giving an estimated excess PTSD cost equal to UAH 14,828 or $507 in 2022 USD. This was assigned to severe PTSD, with lower severities scaled proportionally. Posttreatment costs were assumed to decline 20% per year over five years (Marseille et al. 2020, 2022).
Mortality and Analytic Time Horizon
Using the age-specific background mortality rate in Ukraine as a referent (World Health Organization 2024) we set the relative mortality risks at 1.0, 1.74, 2.05, 2.51, and 2.76 for asymptomatic, mild, moderate, severe, and extreme PTSD, respectively (Ahmadi et al. 2011). The base-case analysis projects costs and health consequences to 3 years. We also report results at 1 and 5 years.
Health State Utility Values
Health State Utility Values. The EQ-5D-5L (EuroQol) questionnaire was administered to the Phase 3 trial participants, and scores were converted to utilities as used in QALY assessments according to the methods outlined in a 2019 study designed specifically to convert EQ-5D-5L scores utility measures (Pickard et al. 2019). Adverse events associated with the trial were transient and are not reflected in the current analysis (Mitchell et al. 2021).
Productivity and Caregiver Costs
With no Ukrainian or European data available, we adapted US estimates of PTSD-related costs. Adjusted for inflation and wage differences, productivity losses for severe PTSD in Ukraine were estimated at $879 in 2022, and caregiver costs at $407, for a combined total of $1286. Costs for milder PTSD cases were scaled proportionally, consistent with healthcare cost adjustments.
Premature Mortality Costs
Premature mortality costs. We calculated the economic impact of PTSD-related early deaths by estimating the number of deaths prevented by MAT and their associated costs. The analysis considered lost productivity based on Ukraine's median annual wage of $6396 (Time Doctor 2023) from age 43 to retirement at 65, adjusted for survival probabilities. We subtracted avoided healthcare costs of $250 annually (2023 prices) (Martsenkovskyi et al. 2024), from age 43 to 89 with costs adjusted downward using Ukrainian life tables for mortality adjustments. All future values are discounted at 3.0%. We applied a 3% annual discount rate and deducted medical costs but not general consumption from these calculations (Rappange et al. 2008).
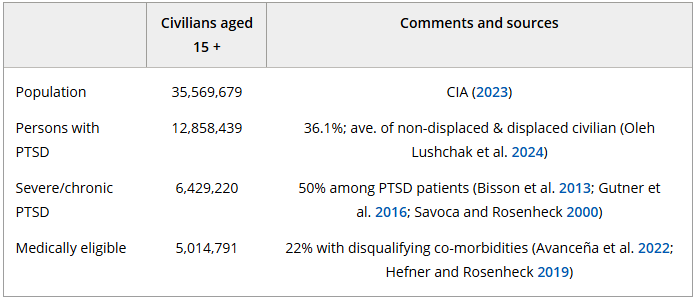
Estimating the Number of Patients Eligible to Receive MAT-AT for PTSD
The civilian population of Ukraine aged 15 and older in 2023 was 35,569,679 (CIA 2023). Of these we estimate that 36.1% have a PCL score of 33+ and thus screen positive for PTSD, assuming the same prevalence among internally displaced and non-internally displaced civilians (O. Lushchak et al. 2024). We adjusted this number downward by 50% to reflect the portion of those with PTSD who are suffering from severe and chronic forms of the disorder, and by an additional 22% to reflect those with disqualifying co-morbidities to reach a final estimate of 5,014,719 (Avanceña et al. 2022; Hefner and Rosenheck 2019). See Table 2.
Estimating the Scaled-up Impact of Access to MAT Over 10 Years
Estimating the scaled-up impact of access to MAT over 10 years. We modeled three illustrative MAT treatment targets: 25%, 50%, and 75% of the eligible civilian population in Ukraine. These treatment targets are based on previous modeling studies on the costs and benefits of scaling up mental health treatment services (Avanceña et al. 2022; Chisholm et al. 2017; Chisholm et al. 2016). For simplicity, we assumed that 10% of the target population would be served in each of 10 years. We did not include estimates of incident cases of PTSD, or of mortality over the 10-year implementation period.
Establishing a Threshold for Cost-Effectiveness in Ukraine
To our knowledge, Ukraine has no guidelines regarding the range of acceptable cost-effectiveness thresholds for its healthcare investments. We therefore estimated a cost-effectiveness threshold for Ukraine based on the ratio of per capita GDP between Ukraine and the average thresholds for U.S., and selected European and Asian countries with known thresholds. These thresholds were provided by a targeted literature review conducted in 2020 (Zhang and Garau 2020). This approach yielded a cost-effectiveness threshold for Ukraine of $5501.
Results
Base Case Results
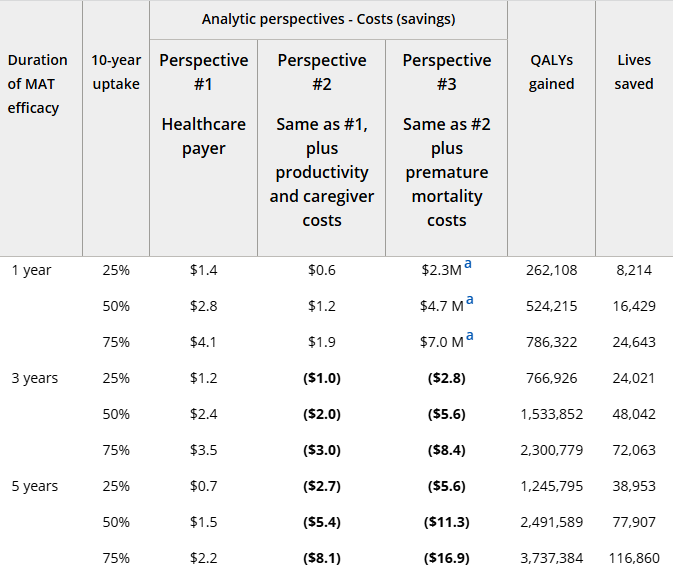
Table 2 displays the results of our analysis for three different analytic horizons 5, 3, and 1 year and from three analytic perspectives: (1) Healthcare payer's perspective; (2) healthcare perspective plus a limited societal perspective that adds productivity gains and reduction in caregiver costs; and, (3) same as 2, but with the addition of the economic gains from reduced premature mortality. Also presented in this section are the results of projected scaled-up access to MAT.
Healthcare Payer Perspective (#1)
From the healthcare payer perspective, treating 1000 patients with MAT over 3 years results in net costs of $1.1M, 717 QALYs gained, and 19 deaths averted. At a WTP of $5501 per QALY, MAT is cost-effective with an NMB of $2843 and ICER of $1537. If benefits last 5 years, cost-effectiveness improves (NMB $5716, ICER $595). If benefits last only 1 year, NMB is near zero and ICER $5261, just meeting the cost-effectiveness threshold.
Limited Societal Perspective That Includes Productivity Effects and Caregiver Costs (Perspective #2)
Given this analytic frame and assuming clinical benefits persist for 3 years, MAT would generate net savings of $933,000. It is the dominant option with an NMB of $4879. If benefits are assumed to last 1 year, MAT retains a favorable ICER of $2,353 and an NMB of $772.
Limited Societal Perspective That Includes Productivity Effects, Caregiver Costs, and Costs of Premature Mortality (Perspective #3)
From this perspective, Ukrainian society saves $2.6 million per 1,000 patients receiving MAT assuming 3 years of benefit. It is the dominant option with an NMB of $6571, and remains dominant assuming only 1 year of benefit (NMB, $1350).
MAT Scale-Up Projections
Table 3 below displays the consequences of scaled-up access to MAT for Ukrainian civilians assuming uptake by 25%, 50%, or 75% of eligible patients with PTSD over 10 years.
For each of the three analytic perspectives and three assumptions about the duration of MAT benefits, the net cost or savings to society are given. Also displayed in this table are the number of QALYs and lives gained given each of the three scale-up scenarios. If 50% of eligible patients received MAT, the net discounted costs over 10 years would be $2.4 billion from the healthcare payer's perspective. A more comprehensive societal perspective would result in net savings of 2.0 billion if productivity effects and caregiving caregiver costs are taken into account (Perspective#2), and net savings of $5.6 billion if economic losses due to premature mortality is additionally included. Assuming 3 years of MAT benefit and uptake by 50% of eligible patients, 1.5 million QALYs would be gained and 48,042 lives would be saved over 10 years (Perspective#3).
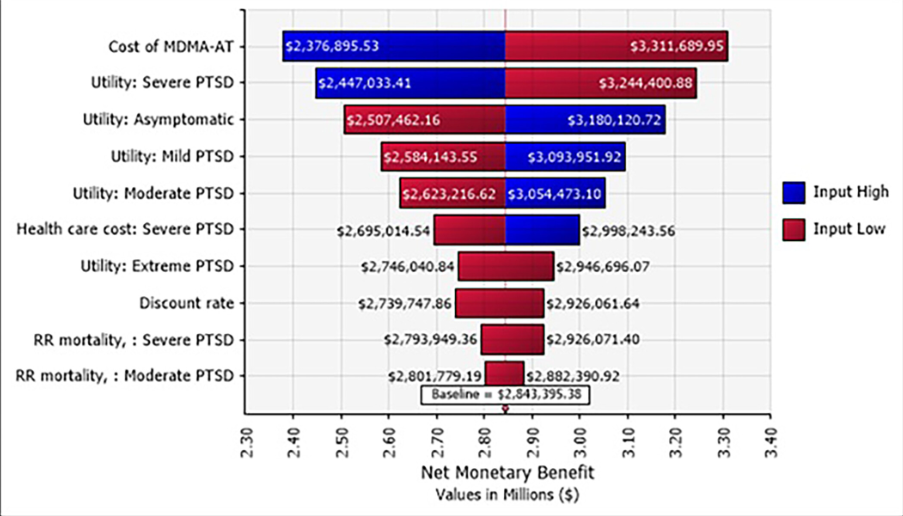
Sensitivity Analyses—Cost-Effectiveness Results
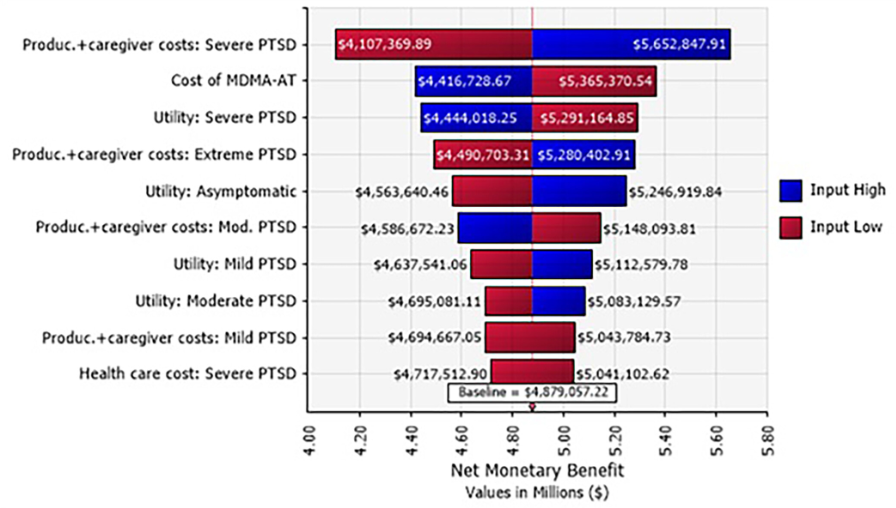
We conducted univariate and multivariate stochastic sensitivity analyses of NMB across three perspectives, assuming 3 years of MAT efficacy.Univariate analysis (Figure 1) shows MAT cost had the greatest impact on NMB, ranging from $2.4M to $3.3M per 1000 patients.
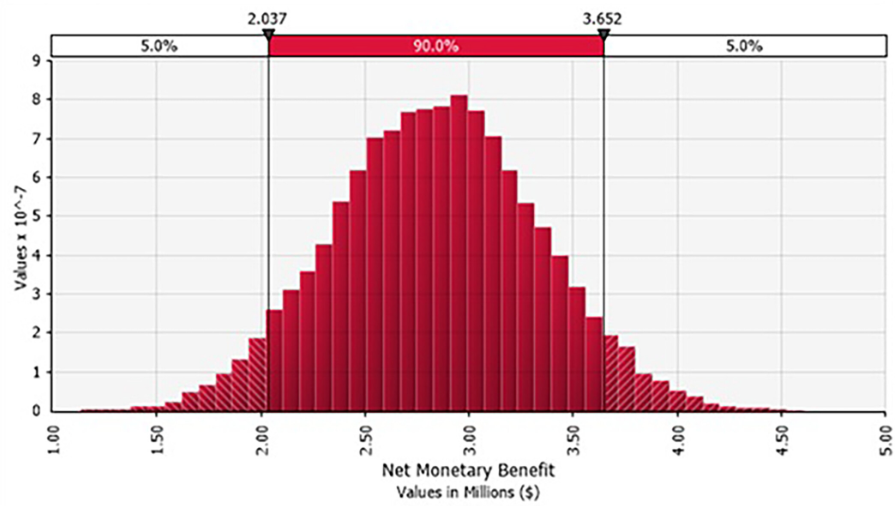
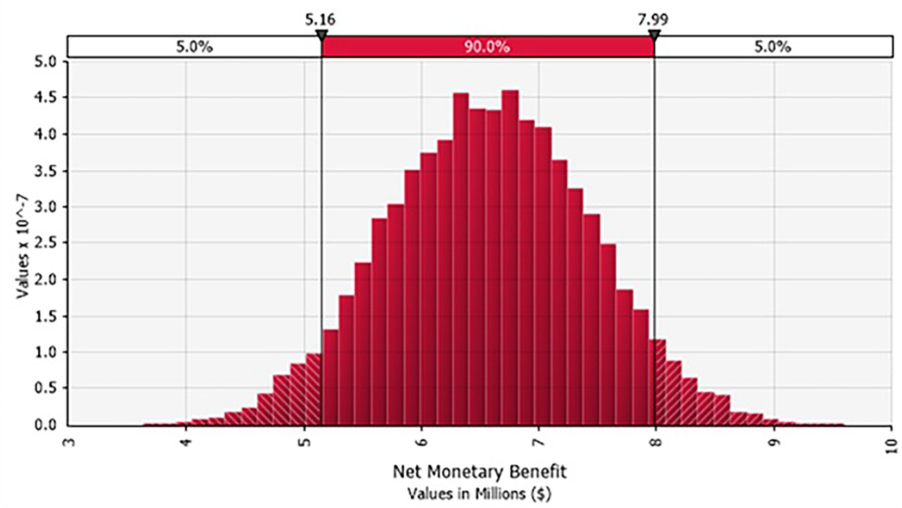
Multivariate analysis (Figure 2) produced a 90% CI of $2.0–$3.7M.
Productivity and caregiver costs for severe PTSD had the largest effect: NMB ranged $4.1M–$5.7M. MAT cost was second ($4.4M–$5.4M). See Figure 3.
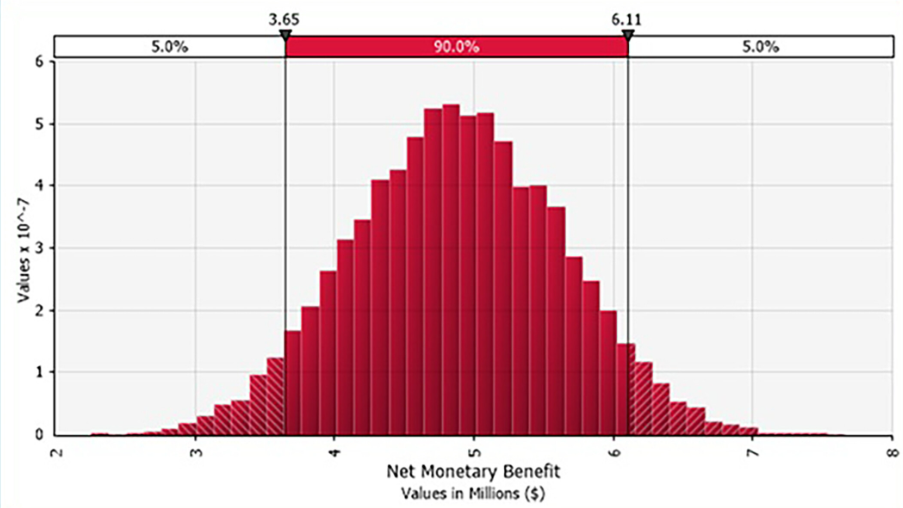
Multivariate analysis (Figure 4) gave a 90% CI of $3.6–$6.1M.
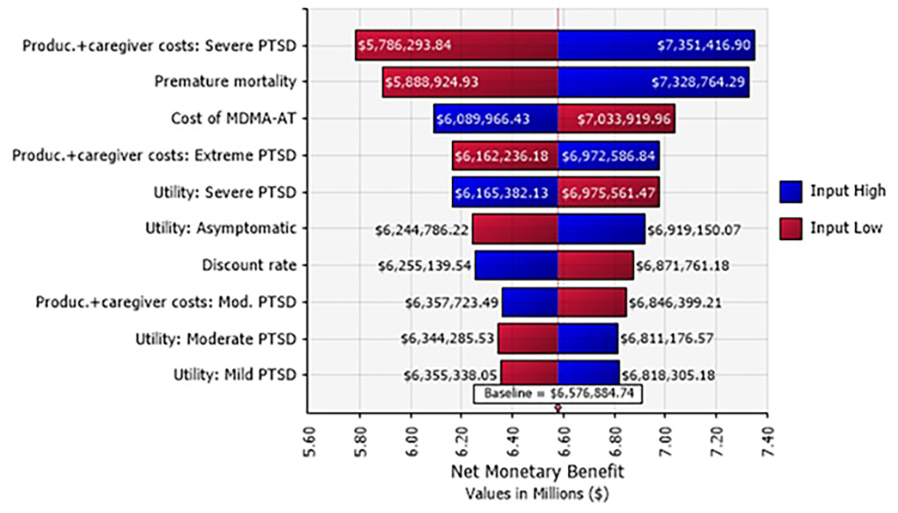
In univariate analysis, productivity/caregiver costs had the strongest effect ($5.8M–$7.4M), followed by premature mortality losses ($5.9M–$7.3M). See Figure 5.
Multivariate analysis (Figure 6) gave a 90% CI of $5.2–$8.0M.
Sensitivity Analyses—Scaled-Up Effects
Assuming 50% of eligible PTSD patients receive MAT over 10 years, with 3 years of efficacy.
Perspective #1Net costs most affected by MAT cost ($1.3–$3.4B). Multivariate CI: $1.3–$3.5B. Lives saved vary 15,000–88,000 (90% CI).
Perspective #2Univariate savings from MAT cost: $1.0–$3.0B; discount rate: $1.8–$2.2B. Multivariate CI: −$4.3B (savings) to $0.3B.
Perspective #3Most influential: premature mortality (−$7.3 to −$4.2B), MAT cost (−$6.6 to −$4.6B), discount rate (−$6.5 to −$4.9B). Multivariate CI: $3.0–$8.4B savings.
Sensitivity Analyses for Willingness to Pay
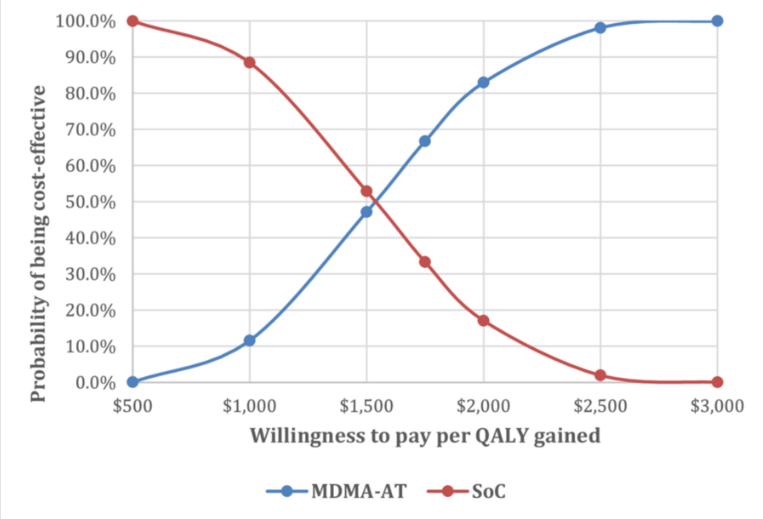
Ukraine’s WTP is estimated at $5501/QALY, though uncertain. With 20,000 simulations (3-year efficacy), MAT is >50% cost-effective at WTP >$1500/QALY, and ~100% at $2500/QALY (Figure 7).
For Perspective #2, MAT is nearly 100% cost-effective at $500/QALY; for Perspective #3 at $0/QALY.
Scenario Analysis—Adding Nonclinical Assistants
Adding peer support assistants (O. Orlov & UPRA 2025) at $6396 annual wage increases MAT costs by 12.4% ($157/patient). For 1000 patients over 3 years, net costs are $1,259,858 (Perspective #1), while Perspectives #2 and #3 yield savings of $775,873 and $2,468,788.
Conclusions
The war has severely damaged Ukraine’s mental health system (Seleznova et al. 2023; Ventriglio & Ricci 2023; Zasiekina et al. 2023). Facility destruction and shortages of medics, especially women (Dzhus & Golovach 2022; Haque et al. 2024), limit PTSD care. Innovative treatments like MAT, with proven efficacy and cost savings (Marseille et al. 2022; Pavlova et al. 2024), are urgently needed.
In March 2025, Ukraine’s Ministry of Health proposed rescheduling MDMA, psilocybin, LSD, and DMT to allow scientific and educational use(Hawrot 2025). In April–May 2025, MAPS and UPRA trained ~60 Ukrainian therapists in MAT protocols (MAPS 2025).
Ketamine remains the only psychedelic legally used for mental health, but reforms could open access to MDMA.
Our study shows MAT is cost-effective even with healthcare costs only: $1.1M net cost per 1000 patients, 717 QALYs gained, 19.2 deaths averted, NMB $2843, ICER $1537 at WTP $5501. In broader perspectives, MAT is dominant—saving costs and improving health—even if benefits end after 12 months (NMB $1350–$11,692 for 1–5 years of benefit).
Given therapist shortages, group therapy is explored to reduce costs and double patient access (Agrawal et al. 2024; Anderson et al. 2020; Oehen & Gasser 2022; Stauffer et al. 2025; Marseille et al. 2023).
Implementation requires training and integration into mental health services, but evidence supports MAT as part of Ukraine’s strategy. Further research should focus on Ukrainian-specific outcomes.
Limitations
We relied on U.S. data for PTSD mortality, severity, and MAT efficacy. The Phase 3 trial excluded group therapy, though early evidence supports it (Agrawal et al. 2024; Anderson et al. 2020; Oehen & Gasser 2022; Trope et al. 2019). Ukrainian patient characteristics differ from U.S. samples. Military personnel were excluded. Productivity gains from reduced disability and broader societal benefits (e.g., reduced violence, accidents, criminal justice costs) were not included, likely underestimating MAT’s value.
Acknowledgments
We wish to acknowledge Amelia Lubelska, Seanne Chan and Isabella Wright undergraduate interns at the University of California, Berkely at the time of their work on this analysis; and Ishaan S. Bhagat at the University of Texas, for their diligent help in reviewing the literature on PTSD in Ukraine and extracting relevant statistics on prevalence and costs.
Conflicts of Interest
Authors conducted this analysis pro bono, with no conflicts of interest.
